BLACK FUNGUS AND ORAL CANCER REHABILITATION
Navigating the complex intersection of oral health and medical conditions like black fungus and oral cancer demands specialized expertise and care. Black fungus, scientifically known as mucormycosis, and oral cancer are serious health concerns that can profoundly affect oral structures and overall well-being. Dental rehabilitation plays a pivotal role in addressing the consequences of these conditions, offering patients a path towards improved oral function, comfort, and aesthetics. Dr Sai Santosh who is our chief Craniofacial surgeon and Advanced Implantologist will dive into the intricate world of dental rehabilitation for individuals impacted by black fungus and oral cancer, exploring the advanced treatments, prosthetic solutions, and multidisciplinary approaches that empower patients to regain control over their oral health and quality of life. Join us on this journey as we unravel the transformative potential of dental rehabilitation in the face of these challenging medical diagnoses.
Black fungus, also known as mucormycosis, is a serious fungal infection that can affect various parts of the body, including the sinuses, lungs, and brain. It has been particularly associated with COVID-19 patients, especially those with weakened immune systems. Early detection and prompt treatment are crucial for managing this condition. Below is a detailed outline of the rehabilitation and treatment steps for black fungus and oral cancer:
- Medical Evaluation and Diagnosis:A thorough medical evaluation is crucial to confirm the diagnosis of black fungus. This may involve a physical examination, blood tests, imaging studies (such as CT scans or MRIs), and potentially a tissue biopsy for definitive diagnosis.
- Hospitalization:In most cases, hospitalization is necessary, especially for severe cases. This allows for close monitoring and immediate intervention if complications arise.
- Antifungal Therapy:Amphotericin B: This is the primary antifungal medication used to treat black fungus. It's administered intravenously and is effective against many types of fungi, including the one causing mucormycosis.
Posaconazole or Isavuconazole: In some cases, especially for those who can't tolerate Amphotericin B, other antifungal medications may be considered. - Surgical Intervention:Debridement: In cases where the fungus has invaded the tissues, surgical removal (debridement) may be necessary. This involves removing the infected tissue to prevent further spread of the fungus.
Sinus Surgery: If the sinuses are affected, surgical intervention may be required to remove infected tissue and improve drainage. - Control of Underlying Conditions:Managing underlying conditions, especially diabetes, is crucial. This includes strict control of blood sugar levels.
- Wound Care and Hygiene:Proper wound care is essential to prevent secondary infections. This includes regular cleaning, dressing changes, and monitoring for signs of infection.
- Nutritional Support:Adequate nutrition is crucial for the body to fight off infections. Depending on the severity of the infection and the patient's overall health, nutritional supplements or specialized diets may be recommended.
- Rehabilitation and Physical Therapy:Depending on the extent of the infection and surgical interventions, physical therapy and rehabilitation may be needed to regain strength and function.
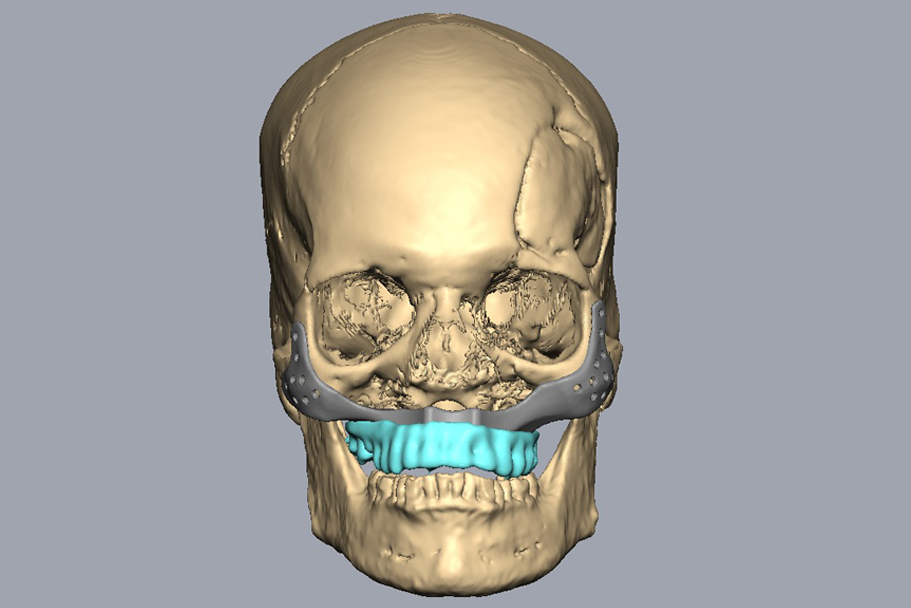
For individuals who have lost multiple teeth, prosthetic options will be considered. This can include partial dentures, bridges, or dental implants to restore function and aesthetics. - Bone Grafting (if necessary):If the jawbone has been affected by mucormycosis, it may require reconstruction through bone grafting procedures. This helps provide a stable foundation for dental implants or other prosthetic options.
- Placement of Dental Implants (if applicable):Dental implants may be considered for individuals with missing teeth. This involves surgically placing artificial tooth roots into the jawbone, which can support replacement teeth.
- Fabrication of Dental Restorations:Custom-made dental crowns, bridges, or dentures are created to match the patient's natural teeth in size, shape, and color.
- Adjustments and Fitting:Once the dental restorations are ready, they are carefully fitted and adjusted to ensure proper alignment and bite.
- Ongoing Monitoring and Follow-Up:Regular follow-up appointments with the healthcare team are crucial to monitor progress, manage any complications, and adjust the treatment plan as needed.
- Psychosocial Support:Dealing with a serious fungal infection like black fungus can be emotionally challenging. Patients and their families may benefit from counseling or support groups to cope with the physical and emotional aspects of the condition.
- Preventative Measures:For individuals at high risk, especially those with weakened immune systems or uncontrolled diabetes, taking steps to minimize exposure to fungal spores is important. This may involve using air filters, avoiding dusty environments, and maintaining good hygiene practices.
- Vaccination and Infection Control:In certain cases, especially for individuals with weakened immune systems, vaccination against specific fungal infections may be recommended. Additionally, strict infection control measures in healthcare settings can help prevent the spread of fungal infections.
It's important to note that the treatment of black fungus should be guided by a team of healthcare professionals, including infectious disease specialists, surgeons, and other relevant specialists. Additionally, individual treatment plans may vary based on the specific circumstances of each patient.
ORAL CANCER REHABILITATION
Oral cancer rehabilitation is a comprehensive approach to help individuals who have been diagnosed and treated for oral cancer to regain and maintain their quality of life. It involves a multidisciplinary team of healthcare professionals, including oncologists, surgeons, dentists, speech therapists, and physical therapists, working together to address the physical, emotional, and functional challenges that may arise after treatment. Here's an overview of oral cancer rehabilitation:
Components of Oral Cancer Rehabilitation:
- Speech and Swallowing Therapy:Speech therapists work with patients to address difficulties with speech, swallowing, and oral motor functions that may arise after surgery or radiation therapy.
- Dental and Prosthodontic Care:Dentists and prosthodontists play a crucial role in restoring dental health after cancer treatment. This may involve procedures like dental implants, dentures, and oral hygiene maintenance.
- Nutritional Counseling:Dietitians provide personalized nutrition plans to help patients meet their dietary needs and maintain proper nutrition during and after treatment.
- Physical Therapy:Physical therapists assist in regaining strength, mobility, and function in the head and neck region, especially after surgery.
- Psychosocial Support:Psychologists, counselors, or support groups provide emotional and psychological support to help patients cope with the challenges of cancer treatment.
- Pain Management:Pain specialists help manage any chronic or acute pain that may result from surgery or other treatments.
- Reconstructive Surgery:Plastic and reconstructive surgeons may perform procedures to restore the appearance and functionality of the mouth and face after cancer treatment.
- Smoking Cessation Programs:For individuals who used tobacco and are looking to quit, smoking cessation programs may be offered to reduce the risk of cancer recurrence.
- Lymphedema Management:Lymphedema therapists can help manage swelling that may occur in the head and neck region after surgery or radiation.
- Functional Rehabilitation:Occupational therapists work with patients to improve activities of daily living, such as self-feeding, oral hygiene, and speech.
- Regular Follow-Up Visits:Patients will have regular follow-up appointments with their healthcare team to monitor their progress and address any new concerns.
- Screening for Recurrence:Regular check-ups and screenings are crucial for early detection of any potential recurrence of oral cancer.
- Individualized Approach:Oral cancer rehabilitation is tailored to the specific needs and challenges faced by each patient, depending on the type and stage of cancer, treatment modalities, and individual health factors.
- Emotional Support:Coping with the physical and emotional impacts of oral cancer treatment can be challenging. Emotional support is an integral part of rehabilitation.
- Holistic Approach:Oral cancer rehabilitation takes into account not only physical recovery, but also emotional, social, and psychological well-being.
- Patient Education:Patients and their families receive education about the potential side effects of treatment and how to manage them.